OSTEOPATH PADDY JOYCE EXPLORES THE DIFFERENT REASONS WE FEEL PAIN AND HOW HE HELPS PEOPLE MOVE THROUGH PAIN IN HIS PRACTICE
As an osteopath the most common reason people come to see me is because they are in pain. Neck pain, Hip pain, Low back pain, Knee Pain…. But what is it??
We often think of pain being the result of an injury: Maybe you’ve torn a muscle, or sprained a ligament. Maybe you might have even broken a bone. However, with pain, this isn’t always the case….
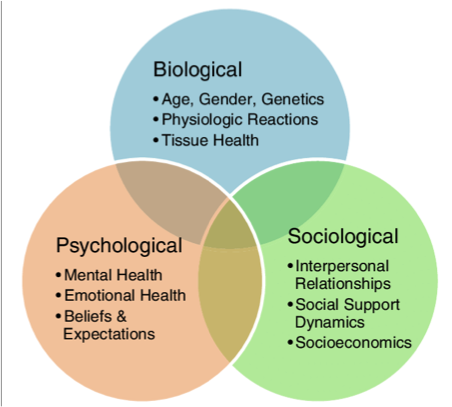
Yes, an injury will usually result in you feeling pain. But it is important to understand that pain is not purely a physical phenomenon. Pain is an interaction between the mind and body, the physical and the emotional. How we experience pain will depend on our beliefs surrounding it, our past experiences and our emotional state, as well as of course the injury itself.
When talking about pain in a diagnostic sense, we tend to categorise it into two main types:
- Acute pain is a severe or sudden pain, or pain of recent onset that resolves within a certain amount of time.
- Chronic pain is persistent, lasting for months or even longer. Chronic pain is considered a health condition in itself.
Acute pain correlates more clearly with tissue damage/injury. We know how the injury was caused, where the pain is, and it tends to get better with time. The purpose of pain of this sort is to act as a warning system, to protect us against further damage.
Chronic pain however often serves no purpose. Our warning system is malfunctioning. Chronic pain does not necessarily correlate with tissue damage/injury and often stays long after the original injury (if there was one) has dissipated. Essentially, there is an error in our pain processing. To understand this phenomenon better it is important to understand how pain is created in our bodies.
PAIN PROCESSING:
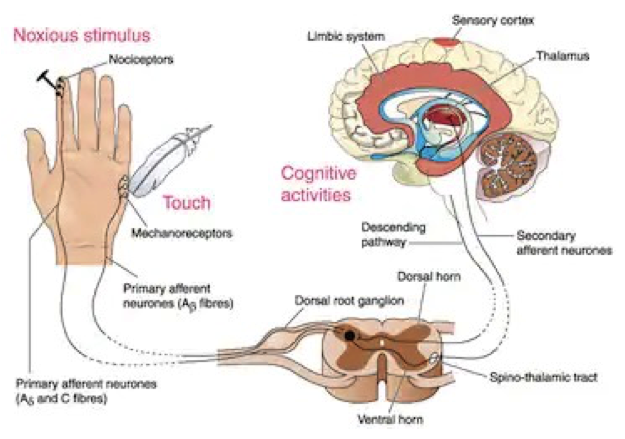
If we look at the pathway for pain (sorry for all the science!), it begins with stimulation of specific types of nerve cells (called nociceptors), which lie in skin, muscles, ligaments, tendons and organs. Like the pin prick shown in the picture. When these nociceptive nerves are stimulated it results in an electrical signal being sent towards the spinal cord along peripheral nerves. If the stimulation is strong enough, chemicals called neurotransmitters will be released, and this electrical signal will be passed further up the spinal cord towards our thalamus located in the brain, and from there to our sensory cortex where the electrical signal is processed.
It’s important to emphasise the word ‘processed’ ! Up until now the stimulus is just an electrical signal. Once it reaches the brain it is then the job of the sensory cortex to decipherer what this signal means. This will depend on a whole range of factors. How strong is the signal? Where in your body has it come from? Is it sharp/dull? Are you stressed/anxious? Have you experienced this before? Are you happy/sad? Based on the answers to these questions and indeed others, it will only be then that your brain determines if you are in pain, and in how much.
Have you ever suffered an injury when you’re on your own? Or in a unfamiliar place? It can feel entirely different in its intensity compared to a similar injury in a familiar environment where there’s lots of help at hand. Have a think about that for a minute or two. Interesting stuff, huh? Its also worth remembering that we evolved our ability to feel pain primarily as a way of protecting ourselves from danger, and from the risk of further injury. So, though it certainly doesn’t feel like it at the time, pain can sometimes be your friend.
FAULTY PROCESSING:
However, this pain pathway I described above can become faulty. Under certain conditions it may become sensitised, meaning pain is felt more readily or with greater consistency. Sometimes this may progress to a point where we feel pain without really any painful stimulus. This can occur if we have previously had negative experiences with injuries or pain, are anxious or depressed, or have unresolved pain for a long duration. At this point our pain can become chronic. When that happens its of little or no use to us.
RESOLVING PAIN:
As I first alluded to, people often come to see me because they are in pain. Perhaps the key role I have as an osteopath is establishing if this pain is acute or chronic, and what factors are at play. Osteopaths take a holistic approach to this, and as such can benefit patients in dealing with their pain to a point of resolution. It may not just be through the physical treatment and advice given, but also through the recognition of psychosocial factors at play in the pain pathway.
If you or someone you know is in pain, pay your local osteopath a visit as they might just be able to help….
If you are interested in exploring the topic of pain further then I highly recommend the following videos:
Professor Lorimer Moseley from the University of South Australia shares a personal story around pain for the exhibit Feeling Human from MOD.’s inaugural exhibition, MOD.IFY. For more from University of South Australia visit: UniSA Homepage: https://www.unisa.edu.au/ UniSA Facebook: https://www.facebook.com/UniSA/ https://www.facebook.com/UniSANewsroom/ UniSA Twitter: https://twitter.com/UniversitySA https://twitter.com/UniSAnewsroom UniSA Instagram: https://www.instagram.com/universitysa/ UniSA Weibo: http://weibo.com/studyatunisa
Prof Peter O’Sullivan discusses some of the myths about back pain which are widely held and negatively impact on the perception and treatment of back pain.
